The American Society of Clinical Oncology (ASCO) is a professional organization representing physicians of all oncology sub-specialties who care for people with cancer. ASCO offers premier scientific events for oncology professionals, patient advocates, industry representatives, and major media outlets worldwide. It is crucial for ANZGOG members to attend to remain informed about the latest global advancements in gynaecological cancer and to build significant international relationships.
Associate Professor Phil Beale, ANZGOG Director has curated a selection of gynaecological cancer highlights from the ASCO meeting held in June, 2024.
A/Prof Beale is the Director of Cancer Services and Director of Palliative Care, Sydney Local Health District, Head of Medical Oncology Department at Concord Hospital, Senior Staff Specialist at RPA, and at Chris O’Brien Lifehouse and Associate Professor at the University of Sydney.
Stay informed on cutting-edge developments in the field through this exclusive compilation.

Contributed by:
A/Prof Philip Beale
Medical Oncologist
ANZGOG Director
ENDOMETRIAL
Long-term Follow-up of Selinexor Maintenance for Patients With TP53wt Advanced or Recurrent Endometrial Cancer: A Prespecified Subgroup Analysis From the Phase 3 ENGOT-EN5/GOG-3055/SIENDO Study (abstract 427956)
Dr Vicky Makker, USA
This study was presented by Vicki Makker and was a preplanned analysis of the Siendo study which has been presented previously. Selinexor prevents the export of XPO1 mediated export of tumour suppressor proteins including TP53. This study was in patients with advanced or recurrent endometrial cancer who had received at least 4 cycles of carboplatin and paclitaxel. They were then randomised to Selinexor 80mg weekly or placebo. This new analysis was done according to treatment allocation and TP53 and MMR status.
The results show a very significant difference in PFS for patients withTP53 receiving Selinexor. The difference 28.4m vs 5.2m was highly significant with a HR of 0.44 and p value =0.0005. For the patients who were p53WT and pMMR the difference was even more marked with median PFS 39.5m vs 4.9m with HR of 0.36. This is in contrast with patients who were dMMR who had mPFS 13.1m vs 3.7m.
The overall survival data from this trial has not reached maturity but in the p53WT/pMMR patients, the trend is very clearly favouring the Selixnor group. The side effect profile has been described previously but does include significant nausea, vomiting and myelosuppression. The QOL/qTWIST analysis favours the Selixnor f=group and is clearly being driven by better cancer control.
These positive results have resulted in a bigger randomised trial in p53 WT patients called XPORT-EC-042 which has opened in Australia and is being run through ANZGOG. This will hopefully confirm a new standard of care in patients with p53 WT pMMR patients leading to improved survival outcomes.
OVARIAN
Phase II randomized multi-centre study of neoadjuvant Olaparib in patients with platinum-sensitive relapsed high grade serous ovarian cancer: The NEO Trial. (abstract 5506)
Dr Stephanie Lheureux, USA
This study was presented by Dr Stephanie Lheureux who is very well known to ANZGOG investigators. The trial was also run at Auckland Hospital with Michelle Wilson as the Principal Investigator at that site. This study looked at the role of Olaparib as neoadjuvant therapy as a marker of sensitivity to the PARPi and therefore opening up the idea of avoiding chemotherapy at first relapse.
The patient population was recurrent platinum-sensitive ovarian cancer who were suitable for secondary surgery. They were given Olaparib 300mg bd for 6 weeks and then depending on response were offered surgery or switching to chemotherapy. 5/41 patients progressed in the initial phase and were given chemotherapy off study. Those patients who continued on to surgery were then randomised to receive chemotherapy followed by Olaparib or Olaparib alone.
Of the 31 who achieved a R0 resection, there was no difference in whether chemotherapy or Olaparib was given as adjuvant therapy. There was a big difference in survival in those who did not reach RO which is consistent with other data from the Desktop studies.
These are very exciting results as the impact on QOL of chemotherapy is well known in these patients and can have significant effects on psychological and physical well-being for the rest of their lives. However, there are many questions still to be answered including the effect of HRD status on the results.
The current standard of surgery for select patients, chemotherapy and Olaparib for appropriate patients in the relapsed setting would need to be tested against this treatment paradigm to be sure chemotherapy can be eliminated without affecting long-term survival. Also, the numbers in this study are small and follow-up time is short. The study also highlights the very important issue of achieving R0 to achieve best outcomes and selecting suitable surgical patients is very important in this setting.
CERVICAL

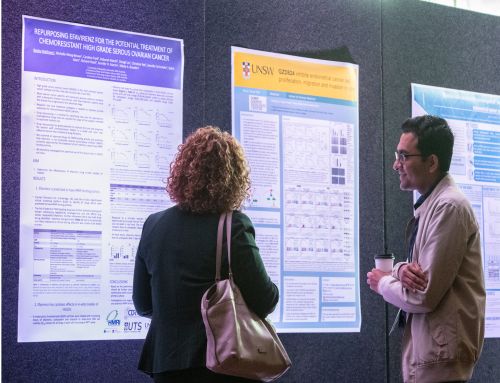
ANZGOG at ASCO: pictured above ANZGOG members Dr Chen Lee and Prof Linda Mileshkin, presenting a poster that analysed the OUTBACK patient data for racial disparities and survival outcomes.
Adjuvant Chemotherapy following Concurrent Chemoradiation (CRT) in High-Risk Early-Stage Cervical Carcinoma Patients Following Radical Hysterectomy: Results of NRG Oncology/RTOG 0724/GOG-0724 (abstract 5504)
Dr Anuja Jhingran, USA
This NRG study looking at the role of adjuvant chemotherapy in patients with resected early cervix cancer was interesting because it complements the OUTBACK study led by Prof Linda Mileshkin and ANZGOG. The patient population was resected early stage (mostly stage 1b) with positive pelvic or paraaortic nodes. They were randomised to either receive standard chemoradiation or CT/RT followed by adjuvant carboplatin paclitaxel. As can be seen from the survival curves there was no difference in the RFS or OS in the two arms. These results are consistent with the OUTBACK study.
There were significant variations in the treatment delivered across the trial with different techniques, different doses and whether brachytherapy was given or not. This highlights treatment variation across the US sites rather than the conclusions of the study.
So, we can conclude that on the basis of this study and the OUTBACK study, there is no role for adjuvant chemotherapy in patients with early cervix cancer treated with surgery or in patients with more local advanced disease who receive chemoradiation.
ANZGOG thanks A/Prof Philip Beale for providing this report for our members. Enjoy more publications, published by ANZGOG members: